When you have fatty liver disease, your liver literally plumps up, inflating with excess fat that your liver cells hoard and store.
Two or three decades ago, the only people who experienced fatty liver disease were chronic alcoholics.
These days, however, more people are being diagnosed with the usually-silent condition; in fact, some doctors say the non-alcoholic fatty liver disease (NAFLD) is reaching near-epidemic proportions.
In fact, according to Pediatric Gastroenterology (Gastroenterol Rep 2016), “non-alcoholic fatty liver disease is the most common form of chronic liver disease seen in children today.”(1)
What’s the reason behind this increase in fatty liver disease diagnoses?
It’s simple: obesity, diabetes, and fatty liver disease share very strong links, and the United States currently is experiencing record amounts of obesity and diabetes.
Therefore, fatty liver disease is occurring more often, too.
Fatty Liver Related To Fat, Not Alcohol
The most extreme form of non-alcoholic fatty liver disease also known technically as nonalcoholic steatohepatitis, or NASH – occurs gradually, over time, as your liver accumulates more and more fat.
When you have NASH, the fat accumulating in your liver eventually causes inflammation and scarring.
Approximately 2 to 5 percent of Americans have nonalcoholic steatohepatitis, according to the National Institute of Diabetes and Digestive and Kidney Diseases.(2)
Up to 20 percent of Americans may have some fat accumulated in their livers, as well, but in their cases, the fat hasn’t yet caused inflammatory damage.
Doctors believe that non-alcoholic fatty liver disease occurs because of insulin resistance, the metabolic problem also at the root of diabetes and possibly heart disease.(3)
When you have insulin resistance, your body’s cells don’t use the insulin you have efficiently to process the sugar in your blood. This may cause an increase in the amount of free fatty acids circulating in your bloodstream, and some of these extra fatty acids may wind up in your liver.
Signs and Symptoms of Fatty Liver Disease Absent
 You probably won’t notice if you have non-alcoholic fatty liver disease – the condition causes few or no symptoms, and most people live with it for years, in many cases without ever realizing they have it.
You probably won’t notice if you have non-alcoholic fatty liver disease – the condition causes few or no symptoms, and most people live with it for years, in many cases without ever realizing they have it.
Symptoms, if they do occur, are fairly nondescript. You might notice some fatigue and possibly some loss of appetite, but if those occur gradually over time, you may not think to mention them to your physician.
In most cases, people are diagnosed with the non-alcoholic fatty liver disease when their physician runs routine blood tests and finds that some of the liver function indicators come back high.
Specifically, tests for aspartate transaminase (AST) and alanine transaminase (ALT) should come back elevated if you have fatty liver disease.
These tests frequently are elevated in perfectly healthy individuals, though, and may not actually indicate a problem. However, if your physician believes you may have non-alcoholic fatty liver disease – possibly due to a physical exam showing an enlarged liver – you’ll need a biopsy to confirm the diagnosis.
Fatty Liver Diagnosed – But What’s Next?
People with diagnosed non-alcoholic fatty liver disease frequently live with the condition for years – often for the rest of their lives – without experiencing problems from it.
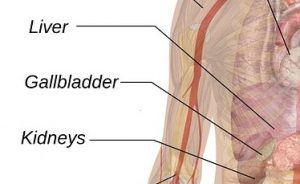
As long as your liver continues to function normally, cleansing your blood of toxins and pumping out enzymes you need for digestion, you shouldn’t notice any effects from the excess fat.
Can Fatty Liver Disease Kill You?
However, in a small percentage of people – it’s not clear how many – fatty liver disease evolves into cirrhosis of the liver.
When you have liver cirrhosis, it means your liver has accumulated so much scar tissue that it no longer functions normally. People with cirrhosis will develop symptoms, including fatigue, loss of appetite, weight loss and weakness.
Once this liver damage occurs, it’s very difficult or impossible to reverse. People with cirrhosis frequently go on to develop liver failure.
In fact, cirrhosis developing from non-alcoholic fatty liver disease is one of the top three reasons for liver transplant operations in the United States. Once cirrhosis develops 30–40 percent of patients will pass away of liver failure over a ten year period.(4)
» find the best products for liver health (Learn more at Amazon)
Preventing or Reversing Fatty Liver Disease
Doctors can’t tell which of their non-alcoholic fatty liver disease patients ultimately will eventually develop cirrhosis of the liver and require a liver transplant.
In fact, there’s been little research to date on the various causes and potential treatments for fatty liver disease – for example, no drugs have been approved.
Although a recent study published in the journal Cell Reports has found promising treatment for NAFLD in laboratory mouse models.(5)
However, it’s possible to make a change in your lifestyle that potentially can reverse fatty liver disease before it progresses to cirrhosis: you can lose weight.
Studies show that losing about 10 percent of your body weight can turn your fatty liver into a normal lean liver.(6,7)
There undoubtedly will be more medical research forthcoming on the non-alcoholic fatty liver disease, especially as the rates of obesity and diabetes rise.
Scientists are studying potential drug treatments, and diagnosis likely will improve.
However, the lifestyle advice – eat better, exercise more and lose weight – should stay the same.
But regardless of what diet program or approach you choose to put your liver on diet , you should consult with your doctor first!
References
(1)http://link.springer.com/article/10.1007%2Fs11894-016-0498-9
(2)https://www.niddk.nih.gov/health-information/health-topics/liver-disease/nonalcoholic-steatohepatitis/Pages/facts.aspx
(3)http://press.endocrine.org/doi/abs/10.1210/jc.2006-0587
(4)AJ McCullough The epidemiology and risk factors of NASH
(5)http://www.cell.com/cell-reports/abstract/S2211-1247(16)30759-8
(6)http://www.ncbi.nlm.nih.gov/pubmed/15842581/
(7)http://www.ncbi.nlm.nih.gov/pubmed/16140415/
Leave Feedback: Was this article helpful?